Psychiatry vs mindfulness: present day science, limitations and challenges
Psychiatry vs mindfulness: present day science, limitations and challenges
We all want to be completely self reliant when it comes to fighting adversity or winning over life struggles. Especially when they affect us mentally. Whether it is simple exam anxiety, sadness due to unknown reasons, grief due to loss of a loved one, trauma due to an accident, or just mental struggles due to daily life challenges, we want this to pass. We want to go back to being our joyous, happy and lighter selves. However rarely, such issues go away on their own. Healthy practises like yoga, meditation, running, strength training or therapy and the support of loved ones do play an important role here and definitely help us get better. But sometimes the issues are deeper, serious and long term and we are made to wonder whether a psychiatric evaluation and/or treatment makes sense.
I have been a mindfulness practitioner for many years (Vipassana meditation), and fortunately started sitting Vipassana courses back in 2001 in India when things were going great in my life. My first few courses were nothing short of life changing and I was in awe of the wisdom that was pouring in through these courses. I moved to US in 2004 and eventually also started volunteering to serve for courses, after finding a strong community of Vipassana in US and seeing how seriously people pursued the path. This went on for more than a decade. However, after that I had to deal with a personal struggle in life and some health issues. And although I was convinced that the path of mindfulness is the panacea to all problems, I also knew it is a slow and arduous path. So I tried to explore and evaluate other paths to wellness in a serious way- yoga (Patanjali tradition), therapy (mostly, Talk therapy, Cognitive Behavioral Therapy and also Mindfulness based Cognitive Therapy). I moved back to India in 2020 and after some persuasion, also tried psychiatry.
While experimenting with all these I had a good opportunity to weigh the benefits as well as limitations understanding their foundational principles, ideologies and philosophies. In this post, I am primarily discussing my understanding and experience of psychiatry as a treatment option from a user perspective and contrasting it with mindfulness. I am not a professional and sharing only based on my own experience and observations. I would also be presenting my opinion based on my discussions with professionals, patients, and from what I have gathered by reading relevant scientific journals and watching acclaimed documentaries. My only intention is to educate others based on what I know while trying to be as objective as possible.
Psychiatry as a body science, not mind science
Quoted in a scientific journal paper- (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2769014)- “Psychiatry is the medical specialty that seeks to help (i.e., assess and treat) people and families living with complex brain disorders including depression, anxiety and other complex disorders, substance abuse disorders, developmental disorders such as autism, and neurodegenerative disorders such as Alzheimer dementia. Traditionally, disorders falling into the province of psychiatry have been those of unknown etiology, and, as researchers have ascertained etiology, some disorders, such as central nervous system disorders, have often shifted to the province of neurology. Now, however, with the tools of modern neuroscience, a deeper understanding of causal pathways to major neuropsychiatric illness is evolving, thus rendering artificial the boundary between psychiatry and neurology. “
Thus, when we say psychiatry, it basically boils down to these two- brain disorders and neurological science.
So the psychiatric approach is to study mental health issues as if they were body issues (brain disorders). It looks at disorders as the physiological, anatomical or pathological manifestation of mental phenomena. This may be somewhat correct but only represents a partial or miniscule view of the human mental universe. A human being consists of both body and mind, as clearly distinct entities. Mind exists as only vibrations- thoughts, logic, feelings, images, sound, voice, smell, taste, language, etc. It is like trying to understand the universe via physics but only sticking to the classical view and not considering any quantum phenomena. The reasons are mainly that we have not yet developed enough scientific methods to measure such subtle phenomena especially those that occur in human mind, like thought or feelings etc. There have been some preliminary studies but they are quite nascent. I may be generalizing, but from a layman perspective, psychiatry in this sense may be good for or limited to visually detectable problems in the brain like tumours, strokes, or any physical abnormalities or a spinal neuro issues. (Most biology, anatomy, physiology, anyways are visual sciences). However for mental phenomena which include thought, intention, feelings, evaluation, analysis, logic, and the senses, we need to include a science that looks directly into the “mind” (mindfulness?).
The chemical imbalance theory and other theories
A long working psychiatric theory for mental disorders has been that everything is caused by a “chemical imbalance” in the brain. That theory is being used a lot by psychiatrists everywhere. However, the scientific community itself has refuted that theory many times. Chemical imbalance in the brain as actually understood in present day psychiatry (https://www.psychiatrictimes.com/view/debunking-two-chemical-imbalance-myths-again)-
“Scientifically speaking, there never was a network of validated hypotheses capable of sustaining a full-blown, global chemical imbalance theory of mental illness. Moreover-and here we come back to Myth 2-psychiatry as a profession and medical specialty never endorsed such a bogus “theory,” when judged by its professional organizations, its peer-reviewed publications, its standard textbooks, or its official pronouncements. Furthermore, the whole notion of some looming, monolithic “Psychiatry” is absurd on its face, as my colleague, George Dawson has argued. To be sure: what many psychiatrists in the 1980s and 1990s did promote was some version of the biogenic amine (or catecholamine) hypothesis of mood disorders, focusing mainly on the neurotransmitters norepinephrine and serotonin…….And, in truth, the significance of serotonin was considerably over-emphasized-owing to what Roger S. McIntyre, MD has facetiously called, “Psychiatry’s High School Crush.” … Most troubling from the standpoint of misleading the general public, pharmaceutical companies heavily promoted the “chemical imbalance” trope in their direct-to-consumer advertising. Indeed, in 1965, Dr Schildkraut stated: A rigorous extrapolation from pharmacological studies to pathophysiology clearly cannot be made. Clinical studies relevant to the catecholamine hypothesis are limited and the findings are inconclusive. It is not possible, therefore, to confirm definitively or to reject the catecholamine hypothesis on the basis of data currently available. The closest thing we have to an “official” position on the etiology of psychiatric disorders is this 1978 statement from the American Psychiatric Association, which was approved by the APA Board of Trustees: “Psychiatric disorders result from the complex interaction of physical, psycho-logical, and social factors and treatment may be directed toward any or all three of these areas.”
Hence, chemical imbalance was never really a theory. It is at best only a “chemical view” of how the disorders manifest during stress or anxiety etc. Moreover, there were three main reasons the theory has been still circulating-
- Mental health problems are very complex and very difficult to explain to patients. In fact, despite a lot of research is being done, psychiatry is still quite nascent and does not know much about the cause of these problems. It mainly focuses on symptomatic relief as does most medical science. The chemical imbalance theory helped psychiatrists “explain” what the problem was to patients in an easy way- You have chemical imbalance in your system. This was also aligned with how medical science normally approaches issues in the physical body as sugar being high or cholesterol being low etc- chemical imbalance. It is important to note this however that “chemical imbalance” has never been tested on any patients- there is no blood work to say one has certain neurotransmitter like dopamine getting fired more than normal etc.
- It helped psychiatrists “sell” the prescription drugs to patients – You have a chemical problem in the body and the chemical we give you will fix it.
- The third reason psychiatrists (especially in the west) stick to this explanation is- to eliminate patient shame. There is a known stigma about mental health issues and people often feel “responsible” and “guilty” for their emotional states etc. There is a view around mental health issues which import that one is not able to manage or control one’s mind and so one is weak or not doing enough which can increase the stress and struggle of the person. So, to free people of this stigma, psychiatrists endorse the view that depression, anxiety, mental health disorders etc are a body problem and hence, there is no reason for people to feel ashamed of themselves. (Found this opinion by multiple psychiatrists on Quora- not sharing the links here as it needs permission)
In essence, chemical imbalance theory helps psychiatrists “explain” what mental illness is to patients in an easy way. It also helps them “sell” the prescription drugs to patients- “You have a chemical problem in the body and the chemical solution we give you will fix it”.
These days there is an upcoming new theory about inflammation as the cause of depression, anxiety etc. There is also a running theory on immunity, that a weak immune system and infection is the cause of mental disorders. Hence, these are all at best, theories. One must understand that a theory is a work in progress and is not the same as scientific fact. Many times people are in awe of science (those who have never studied much science and think of it as some wonder and those who are in the scientific fields but form an ego based view of it). But science is nothing but a set of experiments that try to find the truth of something with a tool that is objective or unbiased in nature. At most, science is a theory in progress while we are trying to make sense of the world. Nothing is final. So too much confidence, especially one that arises either due to ignorance or due to ego, is delusional. One must take everything with a pinch of salt, not encourage blind faith and rely more on one’s own observations (as far as the observations are objective).
References for inflammation and infection theories-
- Inflammatory pathways in psychiatric disorders
- Inflammation in mental disorders: Is microbiota the missing link?
- Inflammation related bio-markers in psychiatric disorders
- Viral infections and schizophrenia
- Viruses and psychiatric disorders
Psychiatry and neuroscience

Psychiatry derives its knowledge from how the neurotransmitters behave during stress, anxiety, depression or other disorders and presents solutions based on a purely neurological perspective (with some understanding of brain structure, organs and functions). It is true that our nervous system is responsible for our thoughts and feelings which is what we deal with on a daily basis. We live in a sensory universe and messaging is central to any mental or bodily function. So focusing on neuroscience is a correct to approach mental challenges. However modern science isn’t still advanced enough to detect neural signals that well and there is no comprehension/detection/understanding of what thought or feeling really constitute. Moreover, so far only a few neurotransmitters have been studied in some detail- primarily acetylcholine, GABA, glutamate, serotonin and dopamine. But in reality there exist more than a 100 neurotransmitters in our system and the how, when and why they are fired is completely unknown. Hence, psychiatry is only able to look with a very limited understanding of what happens inside our mind body sensorium. Additionally, no one’s neurotransmitters levels has ever been tested or measured to really know if there is really any imbalance or deficiency. Many prescription drugs given to patients are related to up-regulation or down-regulation of these neurotransmitters.
No psychiatric tests to evaluate disorders
For example SSRIs (a psychiatric drug like Escitalopram) inhibit the re-uptake of serotonin neurotransmitter at the synapse, thereby making serotonin available for use by the mind. Serotonin is considered an important neurotransmitter and plays an important role in cognition, memory, learning and general body regulation. So taking an SSRI normally leads to better functioning in a depression patient. Similarly, dopamine is another important neurotransmitter which helps us feel pleasure as part of the reward system of our brain. Dopamine dysregulation or over generation is normally considered responsible for psychotic disorders and hence common psychiatric meds for such disorders include dopamine down regulators like Olanzapine or Aripiprazole. However, how much dose each patient needs and whether the depression or psychosis has been caused by the dysregulation of these neurotransmitters is not known or tested and only experimented with in a hit or trial way. This means, when a psychiatrist gives medication to a patient, he only listens to the symptoms and by giving different doses and drug combinations, evaluates the condition of the patient based on what he or she is “feeling”. This is not the same as having a Thyroid disorder, getting Thyroid levels tested in laboratory blood tests and then trying a Thyroxine dose as medication but then re-confirming with another blood test whether the Thyroid levels have become normal post drug use. This kind of testing does not exist in psychiatry so far.
Is body science the right approach for mind?
Another issue here is that medical science of the body is still quite well known and established. We do know the body well enough. However not enough knowledge about how the mind functions and hence making evaluations simply on the basis of how the person is “feeling” may not be accurate enough. What I mean is- mental thoughts and feelings influence each other more easily than body organ functions. As in, while there can be some separation between stomach function and ear function, and meds and treatments can be different for each, there can be very little separation between two different types of feelings. For example, one might feel depressed because one is angry- a person may be feeling angry because there is seemingly no solution for his life’s problem, and feeling helpless for some time can easily trigger feelings of sadness or depression. So even the act of treating a person for a particular type of feeling like anxiety or depression can be error-prone.
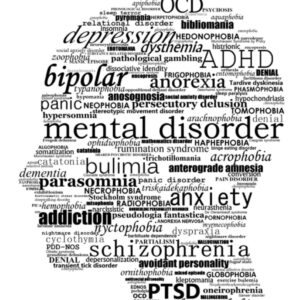
Labelling in psychiatry- stigma and inaccuracy
Psychiatric treatment often starts with an assessment and evaluation based on symptoms and various other factors, and people suffering from mental challenges are given a label of a disorder like PTSD, Bipolar, OCD etc. Many times patients are even labeled with multiple disorders. Now this is similar to what we do in medical science- clustering symptoms together into a disease and isolating a particular set of organs or processes as independent of others and solving only for the problem within that system. For example- blood circulatory disorders, cardiovascular disorders etc. However mental feelings- anger, sadness, grief, frustration etc are more easily connected to each other than body parts since they are vibrations and hence their interaction and impact is quick and immediate. So applying separation in emotions may not be as accurate. Also once a label is assigned, a person starts identifying with it- a label that inherently represents something “bad”- sickness, lack of capability, some kind of craziness etc, which is how mental disorders are often interpreted. Due to these labels, others often start judging and stop trusting you. People even disconnect because they assume there is something “wrong” about you. And it seems like you are not worthy of connection any more. It is both ignorance and judgment that is acting here. Additionally it is also true that most people who have a particular disorder often also have symptoms of other disorders as well. This automatically implies that clustering symptoms into disorders may not be the right approach in the first place. Again goes back to my argument that feelings often arise together and inherently and immediately affect each other. One person never has one particular feeling at any instance, but a multitude of feelings. There are hundreds of different sensations arising in us at an instant due to constant contact with stimuli from the 5 senses and the mind. Hence, treating a person for only one type of feeling like grief (PTSD) or fear (Panic Anxiety Disorder) etc is incorrect. It is also the only reason that creates the stigma. Instead of looking at these mental phenomena as simply what they are, following a cause and effect principle, and trying to understand with objectivity how they arise and pass, medical science is using labels and subjectivity which encourages “judgment” leading to less social support and feelings of low self worth.
Prescription drugs, mode of action and (side) effects
Prescription drugs are unfortunately given for life making one believe that mental disorders are permanent and will never go away. They can be addictive in nature. In my view this is because they force the mind to choose a particular neural pathway again and again as a shortcut over relying on self control or self awareness. This gives the brain an immediate gratification or fix which in my understanding can cause addiction. Most psychiatric drugs suppress awareness and cause addictive or withdrawal symptoms as serious as seizures, jerks, confusion, headaches, drowsiness, sedated feeling, brain fog, memory and concentration issues, sleepiness etc. This may not be the best thing for the brain and we can keep ourselves informed by reading scientific review articles and acclaimed documentaries on the safety and side effects of these drugs and their inappropriate prescriptions-
- Safety and side effects of psychotropic medications (Paper review on problems with psychotropic medications)
- Benzo withdrawal- Ashton manual (A manual written by a psychiatrist Ashton on benzodiazepine withdrawal effects as experienced by many users and how to taper to minimize the effects)
- Inappropriate prescribing (Misuse and over prescription of psychotropic drugs- by American Psychological Association)
- Medicating Normal– a documentary on the negative side of psychotropic drug prescriptions and their side effects
- Dopamine nation– Youtube channel by Professor Anna Lembke (Anna Lembke is an American psychiatrist who is Chief of the Stanford Addiction Medicine Dual Diagnosis Clinic at Stanford University, she has also written a book by the same name).
The alternative path of mindfulness
Can we evaluate mindfulness as an alternative path to mental wellness? It may be challenging. Mainly because mindfulness is an individual path and although can be verified on an individual basis, but cannot be scientifically proven to be effective because we do not have the tools and techniques in modern science yet to measure the mind and its variances. In fact modern science knows very little about the mind. So can it be scientifically verified? Perhaps, no. But it can be individually verified for sure.
A scientific path- objective, observable and verifiable

As explained in my previous post on the science of mindfulness, a scientific method is an objective exploration of a truth. It involves an object to study and a tool that is used for observation. There are two rules for the tool-
- The tool must be objective in nature and not color or bias the reality in any way.
- The tool should be capable of observation. For example to observe radiation coming from space, one cannot use the microscope. Similarly one cannot use a telescope to observe virus or bacteria on a slide. For normal day to day things like color of sky or clouds, using the human eye is considered a valid tool of observation.
In mindfulness meditation, we use mind as the tool to observe the truth of universal principles manifesting through mental phenomena. To do that we first develop the mind in concentration so it is able to be objective. And then we use this concentrated mind to observe so we can understand the phenomena correctly. The steps to develop a concentrated mind are very methodical and are taught as part of Vipassana courses in the form of Anapana practice. Anapana is a technique taught by the Buddha in which we focus our mind on the incoming and outgoing breath, and observe it objectively while remaining nonjudgmentally aware of the thoughts that are arising and passing away. The focus on the breath helps the mind remain focused in the present and detached from the sensory phenomena of thoughts which affect our concentration. Vipassana meditation is a step ahead wherein we observe our feelings without reaction, thus learn to remain detached to our mind body phenomena so we can observe them with clarity.
The non-attachment to thoughts and feelings, is key to any mindfulness practice. It is like stepping back to watch a mountain from far, instead of walking in it. The distance gives us the perspective. Same is with the practice of mindfulness or Vipassana– which means Right View.
Free from all labels and judgment
Unlike psychiatry, there are no labels in the path of Vipassana. It simply means seeing things as they are, without any reaction or judgment. There is no good or bad. It is what it is. This attitude is critical to healing from any difficulty because it is only the incorrect view that is causing us the pain and misery. It is the judgment that this is bad, that creates all the suffering. According to mindfulness, all craving and aversion (aka likes and dislikes) come from a judgmental view of good and bad only and that is the root cause of all disorderliness. If we use the same judgmental attitude to heal, we will just end up being more sick. Because our perceptions are generated from how we understand the universe. Due to our ignorance, we make assumptions, use beliefs or guesses or logic to evaluate a situation as good or bad. And depending upon what our judgment tells us, we take action. That action can be mental- thoughts, feelings or physical- doing. But our perceptions are unfortunately already biased by previous experiences, and so more often than not, we repeat our mental habit patterns of applying the same judgments.
The way out of suffering is the Right View- or the view of non judgmental awareness. The truth is that we must simply we aware of the truth of the present moment and non evaluate it using our perception, judgement and label it as good or bad. With the judgment of good- we are filled with emotions of craving- greed, sensuality which make us want more. With the judgment of bad- we are filled with emotions of aversion- anger, hatred, fear, which make us run from them. Both states of craving and aversion are not preferable. Only a mind that is present, and nonjudgmentally aware of the present moment, without any evaluation of any kind is what is needed. Such a mind generates feelings of bliss and calm and also keep us non attached to the sensory thoughts and emotions, that bring us suffering.
Vipassana – both a prevention and a cure

As one can see above, mindfulness offers prevention from developing any disorderly patterns in mind which arise only due to judgment. With the development of concentration, mind grows in objectivity and hence is able to achieve calm and tranquility. Resultantly, it also becomes very sharp and remains readily in the present moment absorbing information easily. Thus such a mind is free of any mental afflictions. However, if one has developed an affliction, then also one has to practice the same thing. A mental disorder is nothing but a disturbance caused by stirred thoughts and emotions and a mind that believes too much in the sensory world. Once we start training the mind in detaching from thoughts and emotions and then calmly visiting them objectively or nonjudgmentally from a distance, one is able to come out of such disorders. Because the practice of Vipassana or mindfulness is nothing but a re-view of our mental phenomena. Just like I gave the example of watching a mountain from far to develop perspective, we have to do this for curing our minds of afflictions as well. Instead of going into the details (going deep into the forest one will find wild animals and what not), one can step back from the mountain of the mind, and watch from far. Like we do in wildlife sanctuaries. When we observe from far, we can see more and thus really get to understand the true nature of the mind. By doing this, the afflictions slowly leave the grasp of us. But this takes time and practice. And patience.
Impermanence of all disease or disorders
I have already mentioned above the biggest demerit of psychiatry as a field- it takes all disorders as permanent. Because like medical science today it does not deal with cause and effect. It mostly looks at symptoms and tries to find quick fixes so we can be functional in the present. However that comes with a big cost. We have to take psychiatric drugs for life. Mindfulness on the other hand is based on the fundamental principle of impermanence. According to Buddha’s teachings, all phenomena mental or material are impermanent and are bound to pass away eventually. This is the main insight that arises during the practice of Vipassana meditation which gives us the faith to go on. By simply observing with objectivity, we gain the power to dissolve all passing phenomena. Thus Vipassana gives us hope.
|
Sabbe saṅkhārā aniccā’ti |
All things are impermanent |
One must however be pragmatic about understanding the path of mindfulness correctly and develop patience to practice. Because the path of looking inside ourselves with objectivity and honesty is a long and arduous path.
Mindfulness and cognitive psychology based therapy as part of psychiatric treatments
In my humble opinion, psychiatry must integrate mindfulness and cognitive psychology based therapies as part of their treatment offering. Since psychiatry is only a body science, it is important to see it as that and understand that adding mind sciences completes the picture. Some psychiatrists (happens in all fields though) develop an ego about the science and start projecting it as a complete solution to wellness. I have seen this personally on various platforms including various forums and even Quora. However, for the patient (don’t like this label though), it is imperative that he or she understands that any mental challenges (to that matter even physical) arise in the mind only and then manifest in the body. In the absence of this understanding people will just blindly start believing that a drug can fix their suffering and only find themselves deluded in the long run when it doesn’t. This is already happening more often than not. People take psychiatric drugs for 10-15 yrs and then realize nothing is changing or things have become worse and then they have to dig deeper into what must have really happened. This is very unfortunate. In the west like US or UK, there is some trend around integrating psychiatry with mindfulness or cognitive therapy. That does present the whole picture and offers to provide a multi-pronged approach to the solution. In countries like India, psychiatrists do not spend more than 5-10 mins with a patient and simply prescribe drugs. These trends need to change. Also, at the core of it all, people must accept that one’s own mental and physical wellness is one’s responsibility only. Self reliance and self awareness is important, even if we are getting help from others.
Psychiatry in severe cases or certain disorders
Last but not the least, as I have mentioned in the beginning, the science of psychiatry can be used for helping in cases where the disorders may be severe like epilepsy, severe depression, panic anxiety disorders etc. In epilepsy for example the risk of accident is increased as no one knows when the next seizure might come or what might trigger it. Also in such cases, people’s normal functioning is disabled to the extent they may not be able to live a normal life. In many cases, one has to work to provide for family, or has responsibilities etc. And of course, we all need to be financially self reliant. So taking psychiatric drugs in such cases becomes necessary. The drugs do affect the patients positively enough to resume work etc. However, one must see that this is an option that comes with good and bad. Nothing is ideal or perfect in the universe. So one must see it for what it is- simply a treatment that helps in some ways. This is not a cure and what is happening inside the mind due to the drug, no one knows. Even scientifically. So it is important to not look at psychiatric solutions as a panacea or a wonder. Also, in most other disorders like schizophrenia, bipolar, OCD etc, the drugs are not that effective and very few patients show improvement.

Archana Bahuguna
Related Posts
Can mental disorders be prevented?
Vipassana: A Path to Early Detection of Diseases and Mental Disorders
How to approach OCD from a mindfulness perspective
Search
Categories
- Anxiety (1)
- Beliefs (1)
- Breath observation (1)
- Change (1)
- Compassion (1)
- Concentration (6)
- Disease (1)
- Disorder (1)
- Emotions (8)
- Empathy (1)
- Exam anxiety (1)
- Feelings (4)
- Happiness (1)
- Learning (1)
- Limitations (1)
- Logic (1)
- Meditation (5)
- Mental disorders (4)
- Mindfulness (10)
- Narcissism (1)
- OCD (1)
- Pleasing others (1)
- Psychiatry (1)
- Python tools (1)
- Resilience (2)
- School (1)
- Self view (1)
- Social support (1)
- Speed (1)
- Student (2)
- Students (1)
- Teens (1)
- telehealth (1)
- therapy (1)
- Thoughts (6)
- Vipassana (3)
Latest Posts